And so here I finally am; at the end of my initial experiences with cancer: when I was Coping With Cancer. My depression after bowel cancer was, by it’s very definition, after the physical events of this first phase. But, even so, the depression I experienced was as a direct result of my having to cope with cancer in the first place. So I’ll include it here. Besides, the effects of cancer are not limited to the physical, the mental and emotional impact is very real.
I think it’s important to point out that just because I fell into depression after bowel cancer, this does not mean that everyone does, or will. It is, however, relatively common and forewarned, as they say, is forearmed.
In actual fact, the way I ended up with depression after bowel cancer makes no sense. It didn’t then and it doesn’t now: it started with good news…!
I finished the last of my chemotherapy on 19 February 2015. I then had a scan to see what was what. The follow up meeting, to get that scan result, was on April 15th…
And I was given the all clear.
Yay!
I was told that I was cancer-free. Well, what I was actually told was, ‘[your] scan showed no evidence of local recurrent disease or distant spread.’ But you get the idea.
I should have been thrilled. In fact the consultant, who had just given me the news, asked why I didn’t appear to be thrilled. The reason that I didn’t appear to be thrilled was that I wasn’t thrilled. I wasn’t thrilled at all. In fact, I felt dead inside.

Photo by Matt Collamer on Unsplash
While this was a unique experience, at the time, it is less so now. Strange, though is seems, I respond much better to negative news than positive news. A case in point is how I feel now.
My third surgery of this year was three weeks ago, when I had a hemithyroidectomy. This is when half of the Thyroid Gland is removed. The reason that I needed the surgery was that a nodule in my Thyroid had been identified in my last PET/CT scan and tests showed that it displayed follicular proliferation. This meant that there was a 20-33% chance that the nodule was cancerous.
Last Tuesday, I got the biopsy results back from the surgery, and was given the all clear. Not cancerous. This time there was the briefest flicker of relief and happiness and then I simply shut down. Since then, I’ve been fighting a losing battle to stave off depression.
I’m not completely sure that really focusing on my depression after bowel cancer, so I can write this post, is the wisest thing I can be doing right now. But then, I’m rarely accused of being wise. Besides, it needs to be written and, who knows; it might help.
So, back to Spring 2015. I was feeling completely miserable and, after some thought, I wrote the following in my diary:
I’ve always been a bit prone to depression. A lot prone, when I was younger. But, since the stability of marriage and kids old enough to communicate with, the ‘downs’ have been less frequent and less deep.
Understanding that a positive outlook is vital while fighting cancer, I worked very hard at keeping myself cheerful. So, when the great news that I was ‘cancer free’ was presented to me, instead of being elated, I found myself relaxing into a serious come-down from such a lengthy ‘high’.
By May, my wife had managed to persuade me that I needed to get help. This was something of an achievement because… well, this, further, excerpt from my diary will probably explain:
“It’s got to the point that I’ve booked an appointment with my GP to ask for a referral to a shrink. Oddly enough, the acceptance that I need help has made me feel even lower. Doubtless, in no small part, to the fact that I don’t rate the field of psychology or psychiatrists as a profession. So, having to bare my sole to one of these muppets is not something I’m looking forward to because I’m fairly sure it won’t help. I hope I’m wrong.”
In addition to not having much faith in therapy, I’d never liked the idea of taking drugs that alter the settings of your mind. Because they alter the settings of your mind. And taking something capable of interfering with the way I think, the way I process information, horrifies me.
But then I realised; my mind was already messed up from the chemotherapy. I still had Chemo Brain, which was interfering with the way I thought and processed information. When better to take medication that might mess up my mind than when it was already messed up?!
On May 29th, I saw my local GP. He got me to fill out Patient Health Questionnaire PHQ-9. This is a form designed to see how depressed you are, and, therefore, suggest a line of treatment. I scored 13 out of 27 which was in the Moderate area of depression. I was moderately depressed!

He suggested medication. By this stage, I’d already started seeing a shrink and I thought; ‘In for a penny, in for a pound’. And that’s how I ended up on Citalopram for two years!
It’s funny, looking back over my diary, there’s no reference to visiting my therapist. None! And very little mention of the Citalopram, while I was on it. And no mention of Citalopram at all, during 2015. I remember, at the time, deciding to self-edit my notes, to exclude any mention of my inability to mentally cope with my situation.
I think this remains the prevailing attitude in the UK towards mental and emotional problems: they’re simply not talked about. The hangover of the Stiff Upper Lip mindset is still dominant. And this is a problem.
While I accept that problems in the mind are more difficult to pinpoint, I think that’s it’s clear that they exist. Bits of the mind can become damaged or broken. If someone has damaged, or broken, their leg, they’re not expected to just ignore it and get on with their lives. Why then, is that what is expected of someone with a damaged, or broken, mind?
As would be explained to me by my therapist, this damage can be seen during a functional MRI scan. It is real. It should be accepted as such.
With that in mind, anyone struggling to cope with any mental or emotional aspect of their cancer and/or treatment, should not be ashamed to seek help with it. It can help. Especially if you’re more open to the idea that I was.
Because, I was not the ideal patient!
If I was going to see a therapist, then I wanted to make sure that it was someone who knew what they were talking about. So I went for a Chartered Clinical Psychologist with a Doctorate in Clinical Psychologist. I also went for a she, because I find women easier to open up to than men.
The problem is, that getting someone like this on the NHS is virtually impossible. It may be because of the British attitude towards mental health issues not being considered real issues, but the NHS is hugely underfunded when it comes to providing this type of treatment.
So I’d have to go private. And although I did have private health cover, it didn’t cover things like this, as standard. Probably due to the same issues as mentioned in the previous paragraph. Which meant I’d have to pay myself.
And she wasn’t cheap. She charged £80/hour ($100/€90). Now, I’m sure that there are people living in big cities thinking that £80/hour is cheap but I live in the arse end of nowhere and you could buy a sheep for that!

Photo by Benjamin Sander Bergum on Unsplash
Despite all this expense, I was still highly doubtful about the efficacy of psychology, so I decided to removed body language from the equation. I reasoned that by not doing things like crossing and uncrossing my arms and legs, I could not be read. In that way, I had to be heard. It seemed like such a good idea, at the time…
I was, however, utterly open and honest in what I was saying, I was just sitting stiller than normal. I saw her a total of 10 times. And it was both incredibly helpful and somewhat disappointing.
The disappointing aspect was that she didn’t provide me with any tools with which I could help myself. For some time now, Cognitive Behavioral Therapy (CBT), often linked with Mindfulness, seems to be offered as the solution for everything.
Don’t get me wrong, CBT can be very useful. Less so, however, when you suspect you’re depressed because you’re worried that your cancer is going to come back and ruin the lives of your wife and daughters by killing you. Particularly when, the odds are, that some, or all, of that is going to happen in the near future.
Where she was helpful was as someone to offload on, who could give honest, unbiased advice. I also found out what was going on with me, I was suffering from an Adjustment Disorder, which is the inability to cope with a major change in your life. In my case from being utterly focused on dealing with cancer, to being told: ‘Yeah, you’re fine now; you can just get back on with your life.’
One of the biggest problems with being told that I was cancer free was that I didn’t believe it for a minute. My consultant, while being an excellent surgeon, lacked in bedside manner, which meant that I knew that he thought that my ruptured bowel was likely to result in a recurrence in my abdomen. I also knew that the chemotherapy had been virtually ineffective on me, meaning that any small metastases that had been hiding somewhere in my body, were still there. None of which helped with either the adjustment disorder or the depression after bowel cancer.
As well as telling me about the adjustment disorder, the therapist also persuaded me to stop trying to keep my fears to myself and to be more open with my wife. That advice, alone, was worth the money I spent. It’s helped enormously. It’s certainly the main thing I’ve taken away from my therapy: talk to your wife more.
I was trying to protect her, by keeping my thoughts and my plans to myself. But all I was doing was making my depression after bowel cancer worse, which was having a negative impact on her. By trying to protect her, I was actually making things worse for her. And me! Not very wise at all…
While all this soul searching was going on, the Citalopram was slowly taking hold. When you start an anti-depressant, like Citalopram, it takes a number of weeks to fully take hold. Because of this, there’s no ‘light-bulb’ moment when it kicks in. Instead, one day, you realise that you’ve been less emotional for a while.
The way Citalopram worked on me, was that it smoothed things out a bit. Normally, people experience a full range of emotions, over a period of time, which might look something like this:
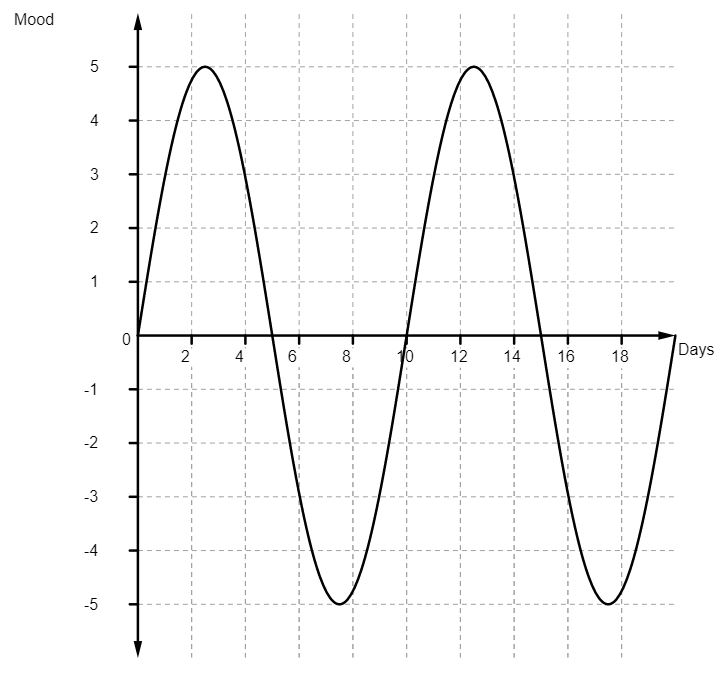
The reality is that the swings wouldn’t be that pronounced or that regular but my technical know-how when it comes to generating graphs only goes so far…
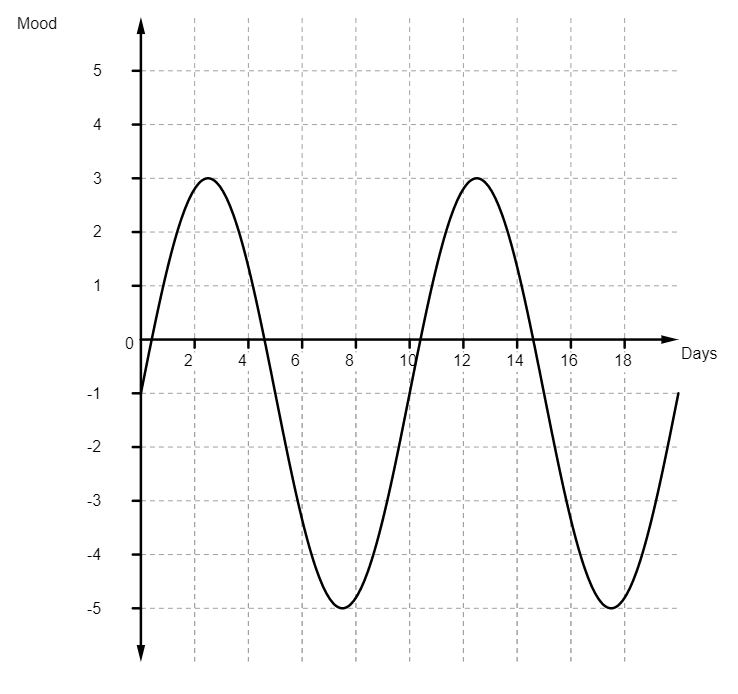
When you’re feeling moderately depressed, you can expect your mood to spend more time under the line than over it, which might look something like this:
What the Citalopram did was something like this:
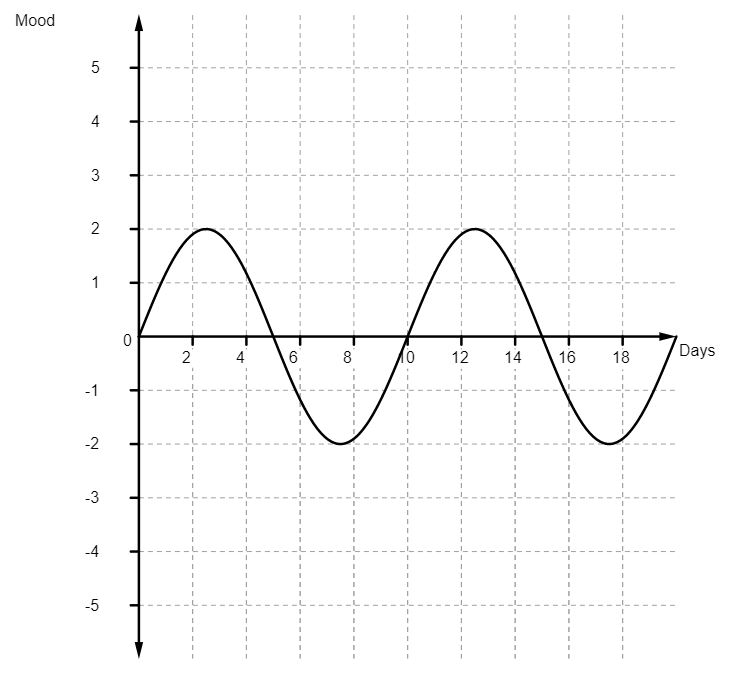
This smoothing out effect was, for me, far from a perfect solution. Fine, I was no longer feeling that depressed but I was no longer feeling much of anything at all. When we went on holidays, I couldn’t raise much enthusiasm. When the girls did something that made me feel proud, I was unable to express this properly.
Fine, I didn’t have the crushing lows but I didn’t have any highs either. Over time, the whole thing started to shift. In was gradual and insidious but, eventually, I realised that my mood graph had become something like this:
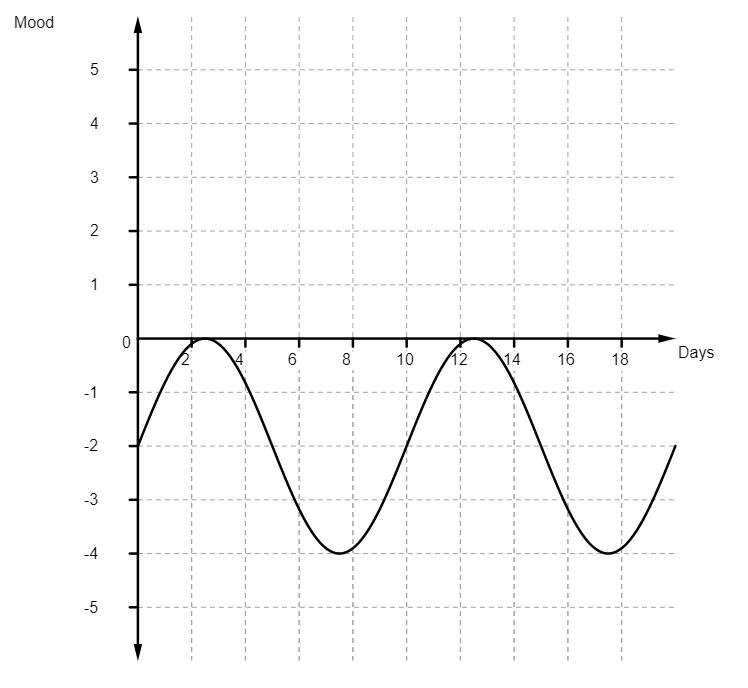
And, while the lows were still not as bad as they had been, on my best days, all I could feel was disinterested. It was at this point that I went back to my doctor and he switched me to Sertraline.
But, before I could start the Sertraline, I had to wean myself off the Citalopram, a process that took a week or so. There would also be an unmedicated period, where the Citalopram had worn off but the Sertraline hadn’t kicked in.
Except I never started taking the Sertraline.
And so, on the 6th January 2017, I stopped taking anti-depressants. In fact, since then, I’ve been completely off prescription medications of any kind. Which I’m pretty chuffed about. As for what happened to my mood, I think my Facebook post of 13th January might help explain:
“Interesting side effect of coming off anti-depressants and getting your emotions back:
You get your emotions back!
But, over the last couple of years and not feeling emotions, I’ve forgotten how to control them now I’ve got them back… it’s like being a bloody teenager again; nought to sixty in a heartbeat.
Poor Julie, she’s now stuck in a house with THREE emotionally unstable teenagers.”
It took a couple of months but I was able to get on top of my emotions again. I’d like to say that I haven’t felt depressed since that time, but that would be a lie. But it’s never been as bad as it was after I was given that initial all clear. And I’m better equipped to handle it now. Depression comes and depression goes. But the important thing is that it does go.
One of the most useful things I saw, while I was battling my depression after bowel cancer, was a World Health Organisation video called, I had a black dog, his name was depression.
This is an amazing watch and resonated so completely with how I felt that it could have been written for me. I strongly recommend it to anyone who is dealing with depression or knows someone who is:
So, there it is.
I fell heavily into depression after bowel cancer. Partly because I succumbed to an Adjustment Disorder after receiving the news that I was cancer free. Partly because I, quite rightly as it turned out, didn’t believe that for a second.
But, just because I became depressed, doesn’t mean anyone else will. But if they do, at least know that you’re not alone. Know also that the depression after bowel cancer doesn’t last forever and that getting help is the right thing to do.
In my case, it took a couple of years to turn the situation around. But, part of the reason that it took so long to get my head around, may well have been the fact that I spent most of that time Living With Cancer. I would have recurrences, more surgeries, more chemo, more gruesome photos…
But, again, just because that has been my experience, doesn’t mean it will be anyone else’s.
And, with this, I end my account of my Coping with Cancer: from the point I found out about it, to the point I put it behind me. However temporarily that was.
Henceforth my posts will be collected under the title that describes my ongoing situation of, Living With Cancer.
8 thoughts on “Depression After Bowel Cancer”
Hi; ran across your blog and wanted to say thank you for sharing your experience. I am in the same boat in Colorado and while I hate for anyone to have to deal with this, knowing you are not alone out there makes a difference. Hope you are staying well!
Hi there,
I’m really sorry to hear that you, too, are struggling with this.
I’m doing okay at the moment, thanks. I hope you are likewise. If you want someone to chat with about anything to do with our respective ‘boat’, please get in touch.
Take care,
Paul
Dealing, with cancer….somehow I could always deal well, almost always deal with everything that came up. Living with the tumor was challenging. I have never had so much trouble dealing with anything as I did dealing with the actual problems the tumor caused. The strange sharp ache in a remote corner of my lower abdomen and back. The weakness, fatigue and just plain tiredness. I felt sick and alone and couldn’t talk to anyone about the problem (still can’t). There was one person I could talk to, my Psychiatrist and she helped me get through the minimally invasive day surgery ( I was out of the hospital in 12 or 15 hours). She medicated me and kept me sane. I needed her and we had a good long run of 12 years. Sadly I couldn’t afford her any longer ($130hr twice a month)so I ended up at the county mental hospital and though they have helped me, medication visits are short and you really can’t talk to them either. So who can I talk to? I feel like you are speaking to me when you write about coping with the emotional and mental pain not to mention the terror around metastasis and recurrence.
I don’t know where I go from here but I do know I have to do something about this tubulovillous adenoma this tumor that has grown through the mesorectal fascia this tumour they got rid of…I have to do something about bowel cancer somehow.
Hi Kayellen,
The reason that I’ve been absent from this site for so long is that I became dressed again, so I can relate with your struggles.
If you want to talk to me, and think I might help, do get in touch.
Paul
Thank you for sharing your experience. It was my husband who just went through treatment for this 4th cancer. The 3rd was bone cancer. They did a stem cell transplant which lasted 3 years. Last year the bone cancer came back. He has now finished a T Cell transplant. I can not begin to explain what I have seen him go through. And truthfully, when he was just given his all clear several months ago, I said nothing. I couldn’t even force out the words, “That’s fantastic!” like I should have. Because I was feeling the same feelings you were. How long will it be gone? Will it or when will it come back, and in what form? No one understands me. I think about this every day. My life is no longer what it used to be. I beat myself up because it is so difficult to be positive and/or happy. I keep my thoughts all to myself. I feel there is no alternative, and therapists don’t give you coping mechanics either. Thank you again for sharing your story. I wish you all the best.
Hi there,
I’m glad to hear that your husband has been given the all clear but so sorry to hear how hard all this has been on you.
“Hammered Flat”, is how I describe the place you seem to be in. It’s like life has taken your thoughts and feelings and just, well, hammered them flat.
It’s an awful place to be and you have my utmost sympathy.
I remember when I was first diagnosed, I didn’t want to talk about anything with my wife. I felt she had enough on her plate dealing with a critically ill husband, without me dumping all my own thoughts and fears on her. In the end, I started keeping a journal. Just for me. And I found it very useful. I was able to write down all my thoughts and fears, to really vent into it when I needed to…
And it really helped me.
Sometimes when I was being squished by the anxiety of waiting to hear the next bit of news, I couldn’t sleep until I’d updated my journal. And the relief of getting it off my mind allowed me to fall asleep quite easily. And, sure, I might wake up earlier than I’d like, worrying about it all again, but it was genuinely helpful. It got me through some tough times.
In the end my therapist, at the time, suggested that I ask my wife if she wanted me to talk to her about things. So, I did ask her, and she did want me to talk to her. But I wouldn’t do it until I knew she had other people to talk to, so it didn’t all end up on her shoulders. She said she could talk to her sister, her mother and a couple of friends, so I felt comfortable opening up to her.
Is there no one close to you that you could talk to, to share what you’re feeling? If not, there are support groups for carers supporting cancer patients. I understand that you feel that no one understands you, but that might be because you’ve been hammered flat and it’s not a good view from down there. I feel that I have some understanding of what you’re going through, albeit from the other side. I feel very confident that there are others out there trapped in the same predicament of thinking that they are alone in their experiences. But we’re not alone.
The colorectal nurses would be good people to ask about support groups. Colorectal nurses are awesome, they know everything.
I do hope you’re able to consider keeping a journal and/or seeking out a relevant support group.
I so hope that you’re able to get back to yourself.
Take care of yourself,
Paul
I obviously do not know you at all, but after reading your excellent posts and following your journey, I cannot tell you how happy I am to see you are still going strong in 2024. I had a friend and brilliant colleague who was diagnosed with advanced colon cancer at age 42. He would tell me prior to his diagnosis of his stomach pains and how his doctors were treating it, etc. Then came the terrible news. He fought hard, yet passed two years later. When he was first diagnosed, I was 38. I completely freaked out and practically insisted that my friend’s gastroenterologist perform a colonoscopy on me. It turned out I was loaded with polyps, some of which were large. Since then, it has been colonoscopies about every two to four years for the past 30+ years. My adult children have been encouraged to get a colonoscopy at age 30. The eldest one had no polyps. The brother that is four years younger had polyps, and is on a more regular colonoscopy schedule. Your posts are well written, pull no punches, honest and encouraging. You describe your ups and downs. So often depression associated with a cancer diagnosis is not discussed, even though it is a heavy weight that poisons what should be happy thoughts and moments. Thank you for what you have done and how you are helping people by enlightening them. All the very best to you!
Hi Jim,
Thank you so much for such encouraging feedback, it means the world.
Sorry to hear about your friend and colleague. It’s good that you were able to turn such a horrible situation into a positive for both you and your children. I’m sure your friend would feel likewise: I know that I would.
All the best to you and your family,
Paul