March 2020 has been something of a roller coaster ride, in terms of what’s going to happen about the tumour in my liver. And, like most people my age who find themselves on a roller coaster, it isn’t much fun!
As you may remember from my February update, after the announcement on the 12th February that I had another recurrence, I was sent for a PET/CT scan. The PET scan took place on the 24th and I had a meeting booked with my oncologist on the 11th March to discuss the treatment options. This was unless I heard from the Spire hospital in Bristol, in the meantime, which would mean that liver surgery was a goer…
So, the wait was on and the nerves were twanging: would I hear from Bristol before the 11th rolled around? Would it be discussions about surgery in Bristol, or discussions about radiotherapy in Taunton? Would the treatment be done by the end of March 2020?
No!
It would be none of those options.
What actually happened was that I got a call from one of the colorectal nurses on the 3rd of March to tell me that the PET scan had revealed, “A bit of uptake in the pelvis.” As a result, I’d need an MRI scan of the pelvis to try and identify the culprit.
Well, that didn’t sound good!
I had the wherewithal to ask some pertinent questions about the location of said hot spot. My first thought was the bone of the pelvic girdle, but I was told it was in the middle of the abdominal region. Do you mean the bladder? I inquired. But, no, apparently it was, ‘out and to the back of the bladder’. It was also not in a lymph node…
I figured that if it wasn’t in the bone, the bladder or a lymph node, how bad could it be, and managed not to get too worried about it. A feeling that was actually helped by the inevitable Google search. And, yes, I understand that Google searches can be problematic, but not if you ask the right question.
The question that I asked led to the following paper:
Frequency and etiology of solitary hot spots in the pelvis at whole-body positron emission tomography/computed tomography imaging
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2743966/
Now that’s a title to behold!
But what it actually is, is a study of 700 patients who have had a PET scan. All 700 are existing cancer patients and all 700 have a solitary hot spot in their pelvis. Frankly, this couldn’t have been more related to my situation, and should have been titled, Oi, Paul, Read This.
The conclusion and results of the study stated the following:
None of the 700 patients was found to have metastatic disease in the pelvis… Isolated pelvic hot spots at PET/CT imaging in an oncological population are not common and usually benign.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2743966/
And, sure, it was only one bit of research, but what a bit of research it was. It was certainly good enough for me not to get worried about what the result of the MRI scan would be.
I was, however, anxious about when the scan would happen. All the discovery of this hot spot was likely to do was delay my treatment, as a potential tidal-wave of coronavirus patients loomed on the horizon.
Because of this concern, I called the colorectal nurse back the following day, the 4th. I asked if there was any chance that the PET scan results could be sent to Bristol, anyway. That way, the Bristol team could assess the liver tumour and be ready to go, if the pelvic hot spot turned out to be nothing. The nurse assured me that my oncologist had already done this very thing…

I immediately blamed my wife, Julie, for pressuring me into making this call in the first place. To be fair, it was her idea. And to be even more fair; if I’m going down, I’m taking someone with me!
In due course, I was told that the scan was booked in for the 11th, which had been the date that I was due to meet the oncologist. Instead, the oncologist meeting got pushed back to the 25th, a full two weeks later. Time really was marching by.
The MRI scan went as well as they ever do and then it was back to waiting and Scanxiety. I cracked within a week and called the colorectal nurse on the 17th, for an update. She had some good news and some excellent news. Maybe March 2020 would be my month, after all!
The excellent news was that the hot spot turned out to be nothing. One of the radiologists had spent ages poring over the individual slices of my scans and managed to build up a picture that showed that the hot spot was being caused by the way I was laying! It seems that a loop of my small intestine got hooked up on my bladder, and the pressure had caused the extra uptake.
Whoever that radiologist is, is a genius to manage to piece that together!
The good news was that Bristol were now willing to look at my CT scans. It seems they’re been waiting on the results of the MRI scan before they were willing to commit. Taunton were already chasing them up for an answer. The main problem was always going to be the timings of the Bristol Multi-Disciplinary Team meeting, which was on a Friday. Meaning I was unlikely to hear anything before Monday. And, as my meeting with the oncologist was on the Wednesday, wouldn’t it be easier to wait until then?
Which is why I wasn’t surprised not to hear anything before my meeting on Wednesday. What I was surprised by was that I was the only patient in the waiting room. I know that the coronavirus pandemic meant that we had to maintain social distancing, but it’s a big waiting room. Another slight surprise was that I never did have that meeting with the oncologist. Instead, the colorectal nurse met me in the waiting room and told me that the Bristol team were happy to go ahead with the surgery.
This, as the nurse pointed out, was really good news. I couldn’t have agreed more if we hadn’t then gone on to discuss the increasing restrictions being placed on hospitals in response to Covid-19. Basically, things needed to happen quickly…
Which is why I got on to my insurance company, the moment I got home. I explained the situation and got authorisation to meet the consultant for discussions about the surgery. The consultant would then give the insurance company the appropriate codes for the surgery, and it’d be all systems go.
Great. Feeling positive. Progress being made. I decided that if I hadn’t heard anything by the end of the next day, I’d start chasing up on the day after (Friday 27th).
As it was, I did hear something on the next day. I got a call from the colorectal nurse checking that the number she was calling me on was the right one. This was because she’d had a call from Bristol saying that they couldn’t get through to me. The mobile coverage at our new house leaves something to be desired. We’re genuinely considering putting in a land line. A landline? Is this March 2020, or March 1920…?!
What followed then was 48 hours of increasing stress levels, as I tried to track down who was trying to contact me. I called the people I thought most likely, but couldn’t get through. I left an answerphone message that elicited no response. [I now know it’s because I was trying the wrong person]
By the end of Friday 27th, I’d got nowhere and didn’t expect that to change over the weekend.
But, I was wrong…
It got worse!
That’s because, on Sunday 29th, I got an email from the consultant who had done all my previous liver resections, which told me that I wouldn’t be having the surgery! Maybe March 2020 just sucked!

Photo by Daniel Herron on Unsplash
The Spire hospital, which is a private facility, was not taking any more bookings for surgeries. It was, in fact, actually cancelling ones that were already in the system. This was in response to an instruction made by Government, during March 2020, to cancel virtually all cancer surgeries, in preparation for said coronavirus tsunami…
Except, that no such instruction seems to exist!
I’ve written a separate post about my thoughts on this policy of canceling the cancer surgeries, so I won’t go into it here. Suffice it to say, I don’t think the decision is justified, proportional or sensible.
The consultant, in his email, said that he’d booked me an appointment with the NHS in Bristol, ‘in order for me to remain in the system’. But he warned me that surgeries in the NHS were extremely limited, and likely to drop off very soon, too.
Well, damn!
My tumour had been at 35 mm when it was picked up by the scan, two months ago…
My best case scenario, regarding the growth of the tumour, was that it had been present in the previous scan, in August, but too small to see. Call it 3 mm. Assuming a steady rate of growth over the course of those six months, that means the tumour is growing at a rate of 50% each month. Alternatively, of course, it could have popped into being at any time during those six months, meaning it’s growing much faster…
But let’s stick with the idea that it was 3 mm in August 2019, and a 50% growth rate. By the end of February, it’s over 50 mm. By the end of March 2020, it gets to nearly 80 mm. Given that I was warned that the 35 mm tumour was sufficiently close to a blood vessel to make surgery tricky, how difficult would surgery be when it was 80 mm? Much more difficult, you’d have to assume.
But now I’m told that surgery isn’t an option. Almost certainly, for the next three months. But probably, in reality, for a number of months more than that. Let’s have a look at what a 50% exponential growth looks like on a chart:
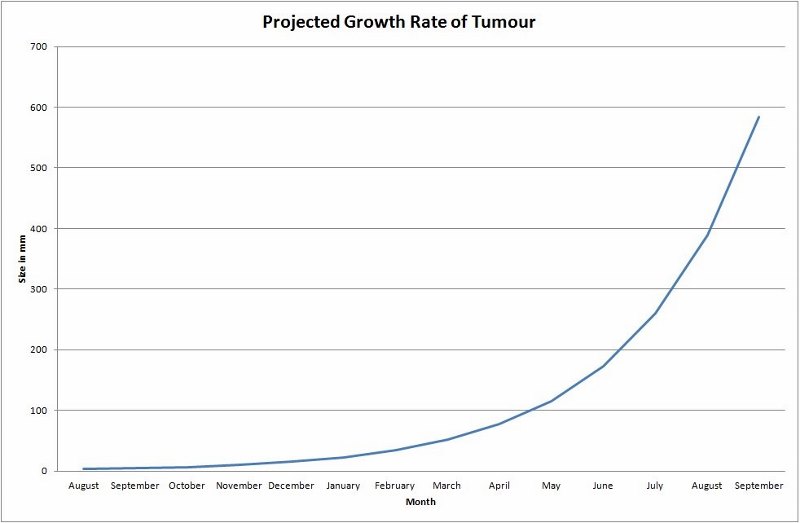
March 2020 also seems to be where things start getting… interesting.
Now, don’t get me wrong, I don’t really think that I’ll have a two foot tumour by September. And, had I let the chart run until December, the projected size of the tumour was nearly two meters…
The reason that I’ve done the graph is fourfold:
- I like maths and messing around with numbers
- To point out that you don’t get two meter tumours, because you die before they get to that size
- To highlight that, while this type of growth curve may not apply to me (hopefully) it will apply to some people
- Some cancer patients are going to die because their surgeries have been cancelled
Now, a cynical person might suggest that history is going to judge Governments by their relative success in dealing with the Coronavirus. And that said ‘success’ will be defined as a lower death rate, per head of population, when compared to similar countries. Such a cynic might then suggest that focusing on Coronavirus cases, at the expense of everything else, would help achieve this favourable comparison. Which, in turn, might secure a re-election…
But, as everyone knows, I’m not a cynical person…
Cough!
Look, I’m really trying hard not to get drawn into my thoughts on cancelling the cancer surgeries. That’s why I’ve split that bit off into a separate post. But I just don’t understand the policy of cancelling treatment before the expected onslaught of Coronavirus patients. That isn’t Triage. There is currently enough capacity to deal with cancer surgeries and Coronavirus. And, given all the extra beds being created for Coronavirus patients, this may remain true throughout the whole pandemic…
It all seems a bit preemptive to me.
And I know what you’re thinking: I’m just selfishly ranting; trying to save my own skin.
Except, I’m not.
I’ve been given an alternative treatment, that doesn’t require surgery. I’ve been offered SABR.
So, while I’m alright, Jack, there are plenty of other cancer patients who won’t be. And, yes, I do feel guilty about this but that doesn’t mean that I’m wrong that cancelling virtually all cancer surgeries at this stage is premature.
Going back to the email from my consultant, it included a referral to another doctor, who specialises in SABR, and the question as to whether I was suitable for that treatment. A glimmer of hope…
And, over the course of the next 24 hours, through a series of emails and a phone call, it became clear that I am suitable for the treatment. Yay! March 2020: how you’ve kept me on my toes!

https://www.kcsn.org.uk/role-of-stereotactic-ablative-radiotherapy-sabr-for-kidney-cancer/
I won’t go in to much detail about SABR, in this post. Largely because I don’t know enough about it. I presume I’ll know more at the end of next month, and can go into detail then. Basically, though, it’s a radiotherapy treatment called Stereotactic ablative radiotherapy. It works by delivering high energy beams through the tumour, thus giving it a really hard time.
SABR is a relatively new technology and only works for some types of tumours. It’s also pretty rare in the UK, and I’m lucky that it’s offered in Bristol. It’s not as effective as surgery but, at the very least, will stunt the growth of the tumour until such time as surgery becomes an option again.
I was told that, given how close the liver tumour is to my stomach, SABR would usually be done under general anaesthetic. With the stomach being laparoscopically held out of the way. But, as that is not an option at the moment, I should expect ‘some inflammation of the stomach’. I think this was his way of telling me that I can expect to be throwing up quite a bit…
Well, at least that’ll make the drive home more interesting. It’s probably just as well the motorway will be so empty…!
And that was March 2020. Like I say; a real roller-coaster ride of emotion and expectation. As it stands, it seems that I have a way through this. It’s not what I hoped for and it’s far from ideal. But it’s a damn sight better than it could have been and, for that, I’m extremely grateful.

2 thoughts on “Progress Update for March 2020”
Well that is fantastic news!!!! Please do let us know how it goes! Hang in there, I trust that you are not yet done with THIS life!! All the best!!!
Hi Cindy,
There’s life in the old dog yet. 🙂
And I’ve got a new and exciting topic to write about…
Take care,
Paul