For me, life after palliative chemotherapy technically started on my 46th Birthday, in September 2016. The scans at the end of my chemotherapy, once again, showed that I was cancer free. As they had done, twice previously. I think it’s fair to say that I didn’t believe that I was cancer free for a second. For a start, it’d been made clear to me that the palliative cancer treatment that I’d been given was designed to debulk tumours, not destroy them. As such the liver and lung tumours that were there before the chemotherapy would be coming back at some point. Which meant I had to prepare for them…
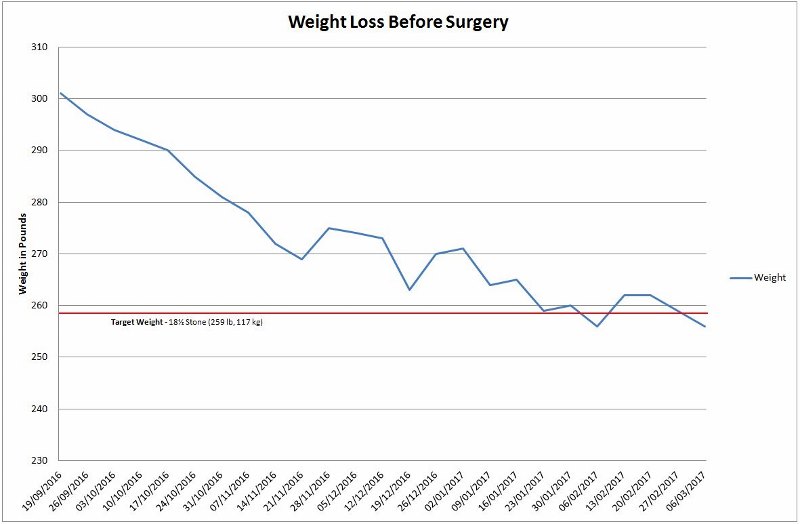
The treatment had not been kind to my health or my body, meaning that I started life after palliative chemotherapy at a pretty low point, both physically and mentally. I weighed around 22 stone (308 lb, 140 kg), which was a personal best! I’d also lost a lot of muscle tone meaning that the percentage of this weight which was made up by body fat was also a personal best. I was breaking records all over the place! Additionally, I’d been on Citalopram for close to 18 months, and that seemed to be helping less. Consequently, I was feeling increasingly low. Finally, I’d had my colostomy bag for the better part of two years, and that was getting old!
To some extent, I’ve covered my life after palliative chemotherapy in two fairly recent posts:
However, these posts are both out of their time; in the Coping with Cancer aspect of the story I was telling. I included them, previously, because they may well fit there for other people going through a similar experience. But that’s not how it was for me and, as I’m recounting my experiences, I feel I need to talk about it here. Apologies for the repetition.
Life without palliative chemotherapy did not start without a pretty solid reminder of life with palliative chemotherapy: the PICC line was still in.
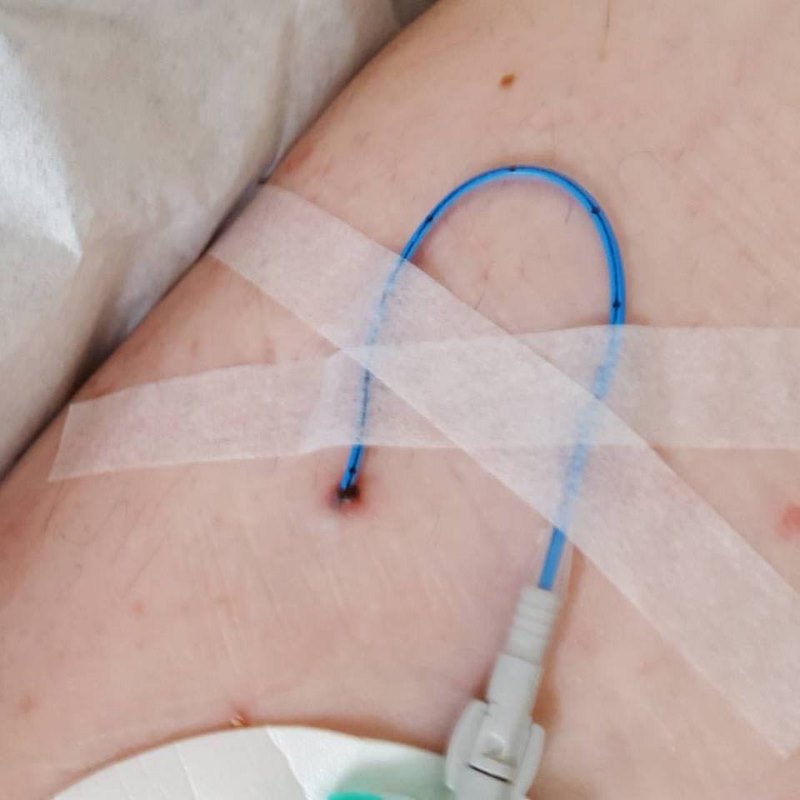
This wouldn’t be removed until after all the scan results came back. Because, if the scans revealed more tumours, I’d probably end up getting more chemo. And there was no point removing it, if they might have to replace it in a couple of weeks. The ongoing physical discomfort of the PICC, tied in nicely with the ongoing mental discomfort of what it meant… Having just gone through six months of Hell, which had left me physically wrecked, I might have to go and do the same again. That prospect played havoc with my mind for a while.
Fortunately, however, I managed to control this emotional turmoil quite quickly. Which was as rare and unexpected as it was welcome. I did this by doing something that I normally try and avoid: I assumed that the scan results would be fine.
To be fair, there was good reason for this; the scans at the half way point showed a reduction in tumour size. But I don’t like assuming the positive, because the psychological crash I experience, when it turns out to be a negative, is all consuming. But, not assuming the positive, would leave me mentally paralysed until I got the scan results. And I needed to start losing weight immediately. So I assumed the positive… and it worked! ![]()
Proof of this success is recorded in the notes from my meeting with the liver surgeon, on September 15th:
He has gained quite a lot of weight in recent months and is now up to 135 kg (21½ stone). However, his stoma and its associated hernia are playing up somewhat to the point it makes it difficult for him to exercise. His mood remains fairly balanced, in part helped by Citalopram.
We have agreed that as the scans are good we can consider stoma closure for him perhaps some time in the New Year, but he certainly needs to lose significant weight prior to that. We have set a target for at least three stones weight loss prior to undertaking surgery.’
What the liver surgeon didn’t know was, despite his horror at my weight, I’d already lost half a stone by this stage. And, while he attributed the balance of my mood to my Citalopram, I had my doubts. I was starting to suspect that the Citalopram was less effective and beneficial than it had been in the past. The liver surgeon also programmed in another meeting for December 1st. He called it a ‘review’ but it was basically to check on my progress with the weight loss.
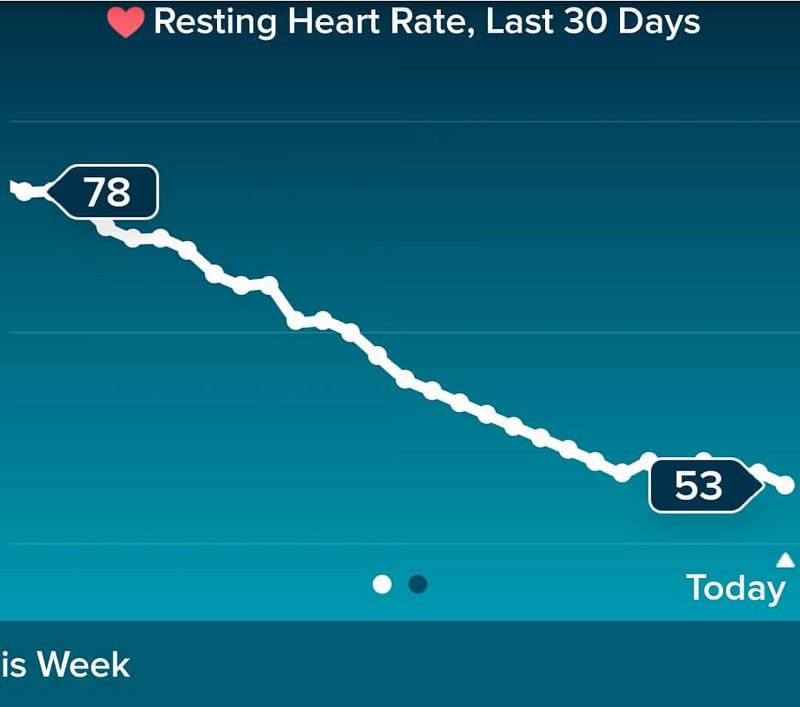
One benefit of life after palliative chemotherapy that I’d already noticed was that my resting heart rate was decreasing. I’d had a fitness watch for some time, in an effort to help my exercise, first a Fitbit, then a Garmin. While I hadn’t been able to exercise much, I did keep track of my sleep and heat rate. My heart rate has always been naturally low. So, when the chemo ended, and my resting heart rate did the following, I was really rather chuffed:
Then it was just a case of waiting for the scan results, which I got by phone. Always a good sign. I recorded this news in a Facebook post, on December 20th, which gives an indication of my mindset at the time:
So, I got my scan results back early and, as expected, the scans found no cancer in my body. And, while this is undoubtedly good news, it marks the start of the waiting game until the tumours reappear. The longer the tumours take to reappear, the better my options for surgery… providing they only come back in one organ.
An additional bit of good news is that my first scans won’t be for six months, instead of the three I was expecting. This could indicate that the Docs are confident that nothing will reappear for a while. Although it could also be because I spoke to my [liver surgeon] and he’s willing to reverse my colostomy early in the new year; and poor scan results at three months might prevent this.
Basically, positive news all round. Including the fact that my biggest concern is no longer dying in a couple of years from cancer, it’s dying in a couple of days from a hockey-induced heart attack. Like it’s supposed to be. 😉
As you can see, while I’m positive and optimistic enough to be dieting, I’m also realistic in my expectations. There is absolutely no doubt in my mind that the tumours will be coming back…
But the next thing that happened was all-out good news. On December 29th, my PICC line came out. It was official; life after palliative chemotherapy was well under way. So I played a full match of (field) hockey on the 24th and didn’t die. I don’t think anyone saw that coming!

But playing hockey wasn’t the main method to help me lose weight, walking was. In actual fact, hockey was more of a hindrance than a help. In a very short space of time, my antics on the hockey field had messed up my knees. Meaning that I was actually exercising less often than I wanted, to accommodate my weekly hockey matches. This might not seem like the most sensible thing to do, but only because it isn’t. On the flip side, playing hockey makes me happy. Being happy means I’m not depressed. Walking every day was fine and the exercise did release endorphins, which improved my mood. But walking every day quickly becomes a chore and chores don’t bolster my mood. Which is why, on balance, I decided to play hockey; even if it did knacker my knees.
I was also dieting quite hard. I tend to do a variation of the Weight Watchers (WW) diet, and this time was no different. With WW, I know that if I only eat the following, each day, I will be inside whatever their current points system allows. Consequently, I will lose weight:
- 80 g of Fruit n Fibre, with 250 ml semi skimmed milk;
- 2 ham sandwiches, on white bread with scraping of margarine
- Home cooked meal, heavy on the vegetables (or WW meals);
- Smoothie of: 120 g banana, 120 g frozen mango pieces, 240 ml semi skimmed milk. This smoothie is a snack that I try very hard to go without when I’m dieting hard, but sometimes I’m so hungry I can’t avoid it.
And, as it always seemed to, the WW and walking plan worked.
It’s actually less effective now (2018) than it used to be. I think all these years of yo-yo dieting have finally broken the WW system for me. I’m currently trying to diet with porridge (oatmeal) replacing the sandwiches and cereal, largely to diffuse the hunger issue… but that’s another story.
By the time I had my review meeting with the liver surgeon, on December 1st, I had made good progress. As the meeting notes recorded:
‘Paul attended for review today. I was delighted to see that he has lost 15 kg, and now weighs 120 kg in his shoes. On the whole he is clearly doing very well… We have therefore agreed to schedule his surgery for the week commencing 20th February.’
Which was conveniently before the dates of my next scans, in March. Oh, it was on!
All this was later confirmed during a meeting with my oncologist, in the New Year. She noted my desire to have the next scans after the scheduled surgery and even went so far as to shift them into April, to make sure this would be the case. Which turned out to be just as well, because, a week later, I got a letter informing me that the surgery would have to be delayed. Probably until early March.
And it was around this time, at the beginning of the year, that I’d finally had enough of Citalopram. At the start, it reduced my depression but also compressed my moods, so they looked something like this:
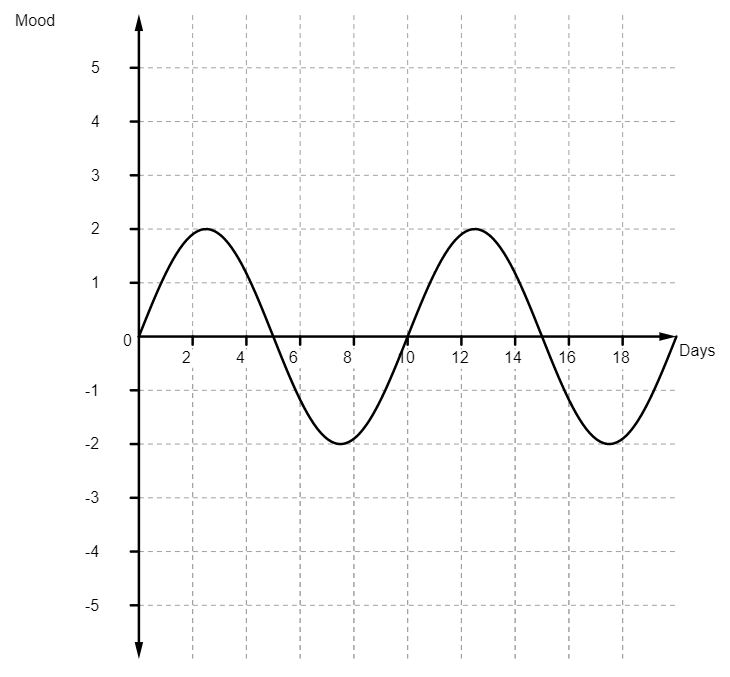
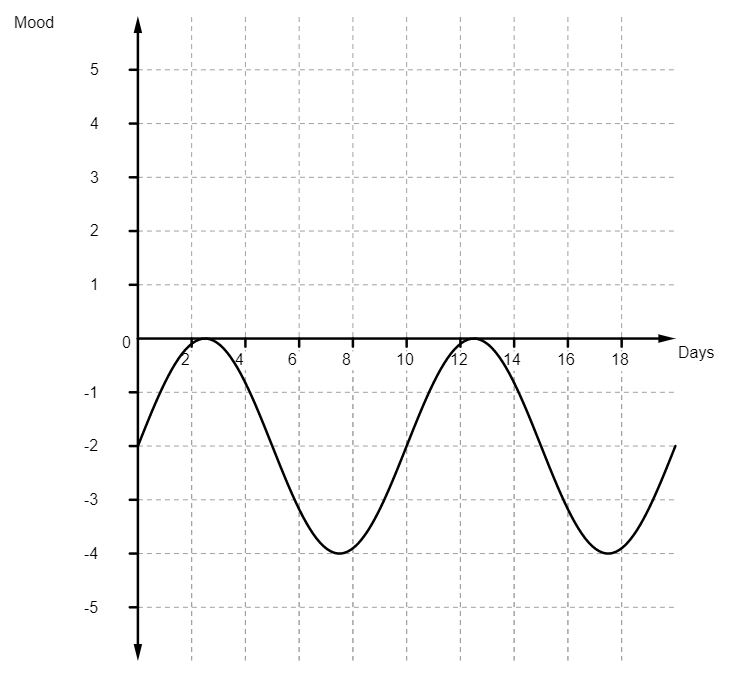
But, by the end of 2016, the whole cycle of my moods, while still compressed, seemed to have shifted to the point they looked something like this:
Life after palliative chemotherapy warranted something better that this. So I went to see my GP and we agreed that it was time to come off the Citalopram. I’d try Sertraline, as a replacement, once I’d weaned myself of the Citalopram. I was warned that there would be a period, while I was switching between the two medications, where neither would be effective. The Citalopram would wear off rather quickly. But the Sertraline would take a couple of weeks to build up to the point that it was effective.
As it was, and bearing in mind that there would be a gap in medication anyway, I decided not to start the Sertraline. I reasoned that if I couldn’t cope without it, I would start taking it then and ride it out. As it was, Friday 6th January 2017 was the last day I took anti-depressants. Yay me!
This, as you can probably imagine, was an interesting time. Probably more for Julie than anyone. When the drug that’s been suppressing your emotions for nearly two years is taken away, your emotions come back. Really quite quickly! It’s like cramming adolescence into two weeks instead of two years. Fortunately, I’d been through adolescence before, so I knew what was happening. Unfortunately, this didn’t help nearly as much as any of the family hoped it might.
There were some stroppy days, in this phase of life of palliative chemotherapy, I can tell you. The slightest irritation escalated to ‘End of the World’ status in mere seconds. Much as my teenage counterpart had, back in the 80s, I spent a lot of time in my room. At least this time, I knew that it wasn’t everyone else that was being unreasonable; it was me. But knowing this didn’t halt the flow of emotions in the slightest, hence the self-imposed exile.
Still, I recovered from the emotional overload in time for the beginning of March, and my reversal surgery. By this stage, I was more than ready to lose the colostomy bag. But, having thought about it for so long, the procedure was very different to what I was expecting. For a start, I didn’t have to take Moviprep, or any other form of industrial strength laxative, to restore my bowel to factory settings.
Nor was there any real talk of the potential need for an ileostomy bag, to allow the colon time to recover before it went back to work. It seems that technology and techniques have advanced sufficiently, in the two years I’d been waiting for the procedure, that such things were no longer a consideration. Advancements such as these are very reassuring to hear about, when you’re receiving palliative care for cancer. It demonstrates that advancements are being made all the time and that new and improved cancer treatments are a very real possibility.

Which meant that my recovery from the reversal procedure was as quick and easy as it could be. Which is to say; quite long and uncomfortable…
You think that learning to reuse your emotions is tricky? Try learning to reuse your butt!
But, relearn it I did. And, in hindsight, it didn’t take too long. Maybe a month, or so. At the time, though, this seems like forever. Laying in bed in an adult nappy, worrying that any fart will lead to disaster. There’s not much sleep involved in those early days. But no one ever said that life after palliative chemotherapy would be plain sailing.
And while my life after palliative chemotherapy might have technically started on my birthday, in September 2016, It actually started, in a meaningful way, on 19th April 2017. Because this is the date that I was told that my scans were clear. The tumours hadn’t come straight back, so I wouldn’t be going straight back on chemo. So, life after palliative chemotherapy had begun.
It was time to get on with living it.
